Besides food, sleep is the most important requirement of every living being, including humans. Sleep refreshes and rejuvenates us, helping our bodies repair and recharge. Sleep stages and sleep cycles play a very crucial role in this process. Whether we are tired, sick, or stressed, sleep heals and re-energizes us.
The process of sleep can be complicated to understand. It isn’t as simple as closing our eyes and dozing off. Several complex processes take place in the brain, bringing about sleep. Our brains work as hard while we are sleeping as when we are awake. Sleep is divided into different stages and cycles. Controlled by the production of hormone regulation, muscle recovery, and memory formation, the primary sleep hormone, the hypothalamus signals the rest of the body if it is time to sleep or to stay awake. Disruption in melatonin production affects the normal sleep-wake cycle.
To understand sleep, we need to understand the different sleep stages and sleep cycles in detail.
What Are Different Sleep Stages?
When we sleep, our brains pass through five different stages, ranging from light to deep sleep. The stages are classified into REM (rapid eye movement) and NREM (non-rapid eye movement) sleep. During the night, our bodies go through the five stages four to five times. Each cycle consists of the five stages. This means, while we sleep, our bodies go through four or five sleep cycles. Each cycle of sleep is roughly 90 minutes long. In an 8-hour sleep, there are four to five 90 minute cycles. In infants and children, each stage is about 50 to 60 minutes long.
Each stage of sleep has an important role in the sleep cycle. All five stages play their own function in rejuvenating and recharging the body for the next day. This includes hormone regulation, muscle recovery, and memory formation. Without enough time to sleep, most of these functions remain incomplete, resulting in fatigue and sleepiness. We might think that only deep sleep is the important stage, but all the stages are equally essential. Without a full night of sleep, the sleep cycle isn’t complete, and the restoration work remains unfulfilled.
Stage 1 of Sleep
Depending on how tired you are, it takes only a few seconds to enter the first stage of sleep, called the transitional phase. This is a non-REM stage, which means the sleep isn’t deep at all. The sleep in this phase is the lightest. People usually flit in and out of consciousness in this stage. If you are exhausted, it will take you only a few seconds to enter the transitional stage, but if you suffer from insomnia or have delayed sleep onset, it can take you an hour or more. Usually, you can still hear everything that’s going on around you and even the slightest noise can wake you up. It is also normal to toss and turn and try to get comfortable. Waking up from this stage is also quick and easy.
In this stage, sometimes your muscles will jerk, jolting you awake. This is called hypnic myoclonia, sleep twitch, or hypnic jerk. These jerks happen because of involuntary muscular contractions. It has been named after the hypnagogic state which is the transitional phase between wakefulness and sleep. Although not all people experience this, they are very common while a person is drifting off. You might even wake up with a start feeling like you were falling. This stage lasts between one and seven minutes. The first stage leads to the second stage of the sleep cycle.
Stage 2 of Sleep
The second stage of sleep is also a non-REM phase, but it is still deeper than the first stage. This phase is when muscles relax, heartbeats begin to slow down, core body temperature drops, eye movements stop, and the person completely drifts off to sleep. Waking up from this stage isn’t as quick as the first stage because the person is making his way to deep sleep. Although this is also a light sleep stage, a person spends more than 50 percent of his sleep in this phase, making it the longest stage in the cycle.
Stage two of the sleep cycle is the precursor to deep sleep. Electrical activity in the brain occurs at a lower frequency compared to the first stage. Brain waves become smaller, with occasional spurts of rapid waves. This phase lasts between 10 and 20 minutes, leading to the third stage.
Stage 3 of Sleep
The third phase can be called the most important stage of the sleep cycle. Lasting between 10 and 40 minutes, this is the stage when sleep is the deepest. During this phase, the heart rate and breathing are at the lowest, and the person has no consciousness of what is happening around him. Waking up from this stage is difficult; if you wake someone up from this stage of sleep, they will remain groggy and disoriented for some time before awakening fully. This stage is also called slow wave sleep when growth and restorative hormones are released.
These hormones have an important role in the development and nourishment of the body. In infants and children, a significant portion of brain and body development takes places at this sleep stage. Besides the growth, these hormones also aid in appetite control. The growth hormones aid in replenishing muscles and tissues that were used during that day, while the hormone leptin suppresses appetite and limits the feeling of excessive hunger. When a person doesn’t get sufficient sleep, leptin doesn’t function well, leading to a rise in the appetite-inducing hormone ghrelin. This is why lack of sleep has a connection with weight gain and obesity
Stage 4 of Sleep
This is also a non-REM phase, but the sleep is almost like a coma. It takes a long time to wake up from this stage. This stage of the sleep cycle is often compared to a comatose state because the heart rate and the body temperature are at the lowest, resembling a person in a coma. Muscle movements don’t occur in this stage, while the breathing is rhythmic. A person usually doesn’t turn or change sides in this stage because the body is completely immobile. This stage lasts around 30 minutes, around when the delta waves are produced.
The delta waves in the brain are associated with relaxation and sleep. Delta waves also enhance the body’s healing abilities. These slow deep waves are responsible for deep sleep. The higher the delta waves, the deeper the sleep. Delta waves are most commonly found in infants because they sleep the deepest. As a person ages, delta waves are produced less. This is also the stage when bedwetting, night terrors, and sleepwalking occurs. Although the causes are unclear, when these instances happen, the person has no memory of them. Even if a person wakes up briefly during this sleep phase, they soon fall back asleep and have no memory of waking up.
Stage 5 of Sleep or REM Stage
This is the final stage in the sleep cycle and the only REM phase. This stage is different from the other sleep phases because this is when the brain begins to get active. Most adults spend around 20 percent of their entire sleep in this REM stage, while newborns and babies spend about 50 percent. In all the previous stages, both the mind and the body are at rest, healing and recharging. But in the REM stage, the mind starts waking up and getting active, while the body is still inactive. The REM sleep stage is called Rapid Eye Movement phase because the eyes move in various directions behind closed eyelids, but the muscles are immobile to prevent the person from acting out dreams.
In this stage, the breathing is shallow and irregular, while the heart rate and blood pressure begin to rise. This is also the stage when dreams occur. That is why most dreams occur in the early morning because that’s the last phase of the sleep cycle. People wake up after the REM stage, and the body temperature comes to normal.
What Factors Affect Sleep Stages and Sleep Cycles?
Although the sleep cycle is made up of these five stages, the cycle isn’t the same in every individual. When the sleep cycle doesn’t take place normally, it results in sleep disorders. There is no certainty that every person will sleep for eight hours or have five sleep cycles. Some people may wake up even before reaching REM sleep. Certain individuals take a few seconds to drift off to sleep while others take an hour or two. This cycle may naturally be a specific way, because of the changes in the structure and function of the brain during development, or may be affected by various external factors.
More often than not, external factors are responsible for regulating the sleep cycle a certain way. Most important among these factors are:
· Age of the Person
Most of us are aware that sleep patterns change with age. Over our lifespan, the amount of time we spend sleeping each day gradually declines. Newborns and infants sleep the maximum, anywhere between 16 and 20 hours each day. Children up to the age of four sleep around 11 to 12 hours. As the child grows up, the amount of sleep keeps declining. An adolescent needs around nine hours of sleep each night, although they may not get that much. Adults need at least eight hours no matter how old they grow, but after middle age, the amount gradually drops. The elderly also need eight hours, but poor sleep quality may not always let them get the full amount at one stretch. That is why those who are unable to get the required sleep at night should make up for it some other time during the day.
The decline in sleep amount and quality has been attributed to the delta waves in the brain. These slow and deep brain waves are responsible for causing deep and sound sleep. When delta waves are higher, the sleep quality is at its best. Because newborns and infants have the highest delta waves, their sleep is the deepest and longest. With age, the slow waves decline. Since REM sleep is known to be important for cognitive development, it isn’t surprising that infants and children spend more than 50 percent of the sleep in the REM stage. As the person grows older, the need for REM sleep also drops. Although sleep problems are a normal part of aging, paying attention to the sleep cycle can help improve sleeping patterns.
· Circadian Rhythm
There is a sleep-wake balancing process that also influences our quality of sleep. We fall asleep only when there is a sleep deficit, and serotonin is acetylated to melatonin. Serotonin is the hormone for relaxation, which helps the body prepare for sleep. It is a precursor to melatonin, the sleep hormone.
This internal, biological clock can vary from one individual to another. Some people may feel sleepy at 8 in the evening while others may stay awake until midnight. Typically, the duration of this biological clock is slightly longer than 24 hours. That is why, the later you go to bed, the later you wake up the next morning. Depending upon the time you go to bed, the body clock adjusts itself. When the adjustment happens naturally, the sleep-wake cycle is free running. Because most humans are diurnal beings, the body clock syncs each day with various external factors like daylight hours, work schedule, etc. The ability of our internal clock to reset according to these factors help keep the circadian rhythm regular and boosts the quality of sleep.
Although this is an internal process, the circadian rhythm is often affected by various external factors, such as working or studying until late, driving at night, or changes in time zones. Jet lag, experienced when traveling across different time zones, takes a toll on the natural internal clock and disrupts the sleep-wake cycle.
· Previous Wakefulness Period
We can fall asleep quickly and easily only when there is accumulated sleep. For maintaining a healthy sleep cycle, this gap between two sleep sessions is extremely important. There was a time in preindustrial Europe when people used to sleep in two phases. This was governed not by a fixed bedtime, but by whether or not there was anything to do. Back then, there was not much to do in terms of work because industries hadn’t yet begun. There was no electricity, so there was nothing to do at home either. Once dusk fell, people would go to sleep for a few hours, waking up late in the evening for an hour or two. After supper, they would go to sleep again till dawn. This bi-modal sleep was prevalent till a long time.
In our modern lifestyles, it isn’t clear whether this bi-modal sleep pattern will work. Sleep starts accumulating once we wake up in the morning. By late evening, when enough sleep has accumulated, we start to feel tired and drowsy. This indicates that our energy resources are depleted, and we need to recharge. If the gap between two sleep sessions is too small, sleep doesn’t accumulate enough, resulting in delayed sleep onset. That is why people who suffer from insomnia are discouraged from napping because sleeping in the middle of the day shortens the time between the two sleep sessions. The longer you go without sleep, the more your sleep deficit.
· Ambient or Environmental Factors
Our surroundings play a key role in our sleep cycle. Environmental factors are often among the biggest causes of sleep disorders, although they usually go undiagnosed. The temperature of the room, ambient noise, light, comfort of the bed, and electronic distractions play a crucial role in the ability to fall and stay asleep. It was found in several studies that those who live in a poorer underprivileged neighborhood are more likely to suffer from sleep issues because of environmental distractions. Passing vehicles till late in the night, noisy neighbors, talking and screaming, loud music and TV, as well as an uncomfortable bed and improper temperature of the room, affect the quality of sleep.
Ambient noise is the greatest environmental factor affecting sleep. From the low hum of the fridge to the ticking of the clock to the TV in the next room to noisy kids upstairs, noises can keep you up at night. An uncomfortable bed is also a potential cause of sleep issues. The wrong mattress, a bed that’s too small, or sheets that cause friction are some of the factors. The type of climate we live in also plays a role in regulating our sleep cycle. Extremely cold regions get a little sun, and people living in such a climate produce more melatonin in response to the low light. Those living in warmer regions are more alert and awake because of constant sunshine and less melatonin production. If not removed, many of these environmental distractions can cause serious sleep disorders in the long run.
· Stress and Medications
Among other factors that affect the sleep cycle is stress. The stress hormone cortisol is famous for suppressing melatonin production. The higher the level of cortisol, the lower the level of melatonin. The lower the production of melatonin, the poorer your quality of sleep and the higher the production of cortisol. This vicious cycle often has no end if the person fails to address the stressors and lower his level of stress. Unless cortisol is low, melatonin production will not be sufficient. Chronic stress can lead to insomnia, depression, anxiety, and even cardiac problems.
Certain medications, such as beta blockers (given for high blood pressure) and immunosuppressants can lower the production of melatonin and cause sleep disorders. Medications for blood thinning and heart arrhythmia block the neurotransmitters responsible for the production of melatonin. Those who take such medications regularly are also given sleeping aid to counter any sleep issues.
Aside from medications, alcohol, smoking, and other such addictions also suppress the production of melatonin and cause sleep disorders. Artificial light from electronic devices also causes sleep disorders. This is why those who stay in front of the computer for long hours often have difficulty falling asleep because too much of light suppresses melatonin production. Using the phone before going to bed, reading on a backlit device, or keeping a night lamp on contribute to melatonin suppression.
How To Improve Sleep Quality?
External factors affect sleep quality to a great extent, but much of it could also be genetic. If genetics is the driving factor, there isn’t any way to change them, but external factors can always be changed or removed to restore normal sleep. If the sleep cycle is affected by any underlying medical condition like snoring or sleep apnea, then they cannot be cured by making a few external changes. Such sleep disorders require proper diagnosis and treatment.
If you know that your sleep keeps getting disrupted because of ambient factors, there are several steps you can take to minimize the distractions and restore normal sleep.
· Create A Sleep Cocoon
Your bedroom should be synonymous with sleep; avoid using it for other purposes like working or eating. This is difficult if you don’t have much space in the house, but if you can help it, avoid making your bedroom your office or entertainment corner as best as possible. Make your bedroom your sleep cocoon so that the moment you enter the room, your body gets into relaxation mode. This can be done by removing distractions like electronics, putting up blinds or curtains to keep out ambient lights, prepping the bed. You may also paint the room in a soothing shade, decorating the walls with pictures that make you feel happy and relaxed. Using essential oils like lavender will banish odor and also calm and relax you.
Choose the Right Kind of Mattress
If you have never taken a hard look at the mattress you sleep on, now is the time to. More often than not, people spend most of their lives sleeping on the wrong mattress. Even though the bed is such deeply connected to our sleep quality, we hardly ever stop to notice if we are comfortable enough. A mattress that’s old, worn out, too hot or too cold, too soft or too firm can do more than just ruin your sleep. Sleeping on the wrong mattress for a prolonged period can have far-reaching effects on your health, causing aches and pains in various parts of the anatomy and even leading to serious conditions like cervical spondylitis.
There are several mattress choosing guides available online that help you pick the right mattress depending upon your body weight, sleeping position, and other factors like whether you sleep hot or cold. Depending on the company you choose, you could also have a mattress customized for your needs. Memory foam, innerspring, and latex are some of the popular mattresses today, and they come in various firmness levels. Some are more comfortable than others, but you can always make use of the trial period to find the mattress that suits you best.
· Avoid Screen Time Before Bed
At least two hours until bedtime, reduce the time you spend in front of a backlit device such as TV, phone, tablet, or computer. If possible, also avoid staying in brightly lit rooms before you go to bed. The lesser you expose yourself to artificial light, the more melatonin is produced, aiding in better sleep. While getting up at night, avoid switching on the lights in the room. Either use footlights or keep a small flashlight handy. Switching on lights in the middle of the night reduces your ability to fall back asleep.
· Cut Down Caffeine, Alcohol, and Tobacco Consumption
As already discussed, certain substances like caffeine, tobacco, and alcohol block the neurotransmitters responsible for producing melatonin and make us stay alert and awake. Consumption of these substances close to bedtime has been found to aid in sleep loss and insomnia. Even if you smoke or drink at other times of the day, try to avoid it in the two hours leading to bedtime. Avoid all the things that boost metabolism and hinder the production of melatonin close to bedtime, including exercise and other activities that increase your heart rate.
· Block Ambient Disturbance
If you live in a noisy neighborhood, it can be a potential cause for disrupted sleep. Footsteps above your head, honking vehicles outside your house, or loud music next doors can cause significant distress. You can take measures to prevent this from turning into a nightly affair. Insulation against noise is one of the best solutions against ambient noise. Soundproof glass, carpeting, thick curtains lined with wool, and foam insulation for the walls are some of the measures. If all else fails, consider getting a white noise machine, which drowns out ambient noise by playing some pre-recorded sound like rainfall or ocean waves.
· Improve Sleep Hygiene
Sleep is all about routine. Going to bed and waking up at the same time every day, using crisp clean and comfortable sheets, keeping the room clutter free and well ventilated, and avoiding a heavy meal before bedtime are some of the sleep hygiene measures that can improve sleep quality over time.
Understanding the sleep cycle is often the first step to better sleep quality. When you know, what affects your sleep cycle, you can take measures to cut out distractions and get ample restful sleep every night.
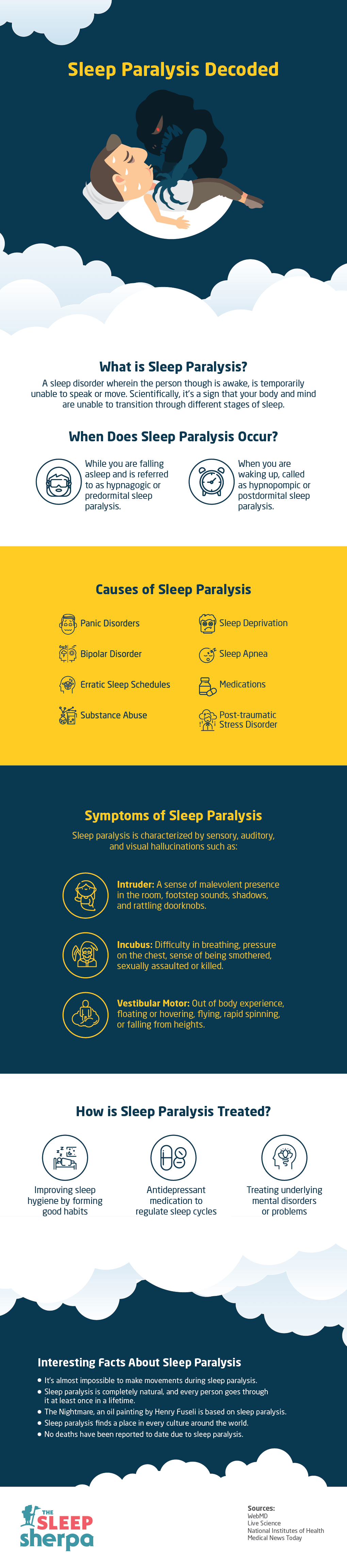
Also, to help you understand the various sleep stages and sleep cycles easily, we have also created an infographic for this.

Infographic Content –
Understanding Stages of Sleep and Sleep Cycles
What Are Sleep Stages? – Characteristics of brain and body defined by brainwave frequencies, and eye and muscle movements. Divided into Rapid Eye Movement (REM) and Non-REM stages.
What is a Sleep Cycle? – The time required to complete five stages of sleep. Typically, it is about 90-120 minutes in an adult, and 50-60 minutes in infants. Four to five sleep cycles per night.
Different Sleep Stages Explained
Stage 1
- Takes seconds to minutes to slip into this stage
- Decreasing heartbeat, breathing, and eye movements
- Transitional phase, relaxed wakefulness before mind begins to drift off
- Easy to wake up, characterized by muscle jerks leading to falling sensation
- Typically Lasts one to seven minutes
Stage 2
- The sleep stage before you enter deep sleep
- Lasts 10 to 25 minutes
- Brain waves become smaller with the occasional burst of rapid waves
- Body temperature drops, eye movements stop and heart rate lowers further
- An average adult spends 50% sleep cycle time in Stage 2
Stage 3
- Deep sleep stage
- Last around 10 to 40 minutes
- Heart rate, breathing is at lowest levels
- Muscles are relaxed; difficult to wake up during this stage
- Body repair, bone and muscle building, immune strengthening occurs
Stage 4
- Coma-like sleep
- 10 to 30 minutes are spent in this stage
- Rhythmic breathing and heart rate; muscle movements extremely limited
- Brain produces delta waves
- Night terrors, sleepwalking, bedwetting can occur in this stage
Stage 5 or REM
- Final stage of sleep cycle where dreaming occurs
- Around 20% time spent in this stage, may last for one to five minutes
- Characterized by rapid side to side movement of eyes behind closed eyelids
- Breathing, heart rate, blood pressure are near wakeful levels
- Arms and muscles paralyzed to prevent body from acting out dreams
Factors that Affect Sleep Cycles
- Age – Infants sleep most while as you age, the requirement decreases gradually
- Gap between previous sleep session
- Internal body clock and its relation to day or night
- Certain medications, exercise, smoking, caffeine, screen time
- Temperature, light and ambient sounds
Controllable Factors to Improve Quality of Sleep
- Ensure bedroom is free from strong smells, dimly lit, and temperature set to comfort
- Get a mattress that suits your sleeping style
- Avoid screen time, smoking, exercising or consuming too much food
- Soft and cool sheets on mattress
- Insulation from noisy environment or use white noise machine
Sources