Sleep apnea, a chronic sleep disorder that affects millions worldwide, has been extensively studied over the years. Traditionally, it has been seen as primarily a men’s disorder. However, emerging research suggests that it affects a significant number of women, too, often undiagnosed due to different symptoms that are misinterpreted (1). As such, the importance of recognizing sleep apnea symptoms in women is increasingly highlighted within the medical community.
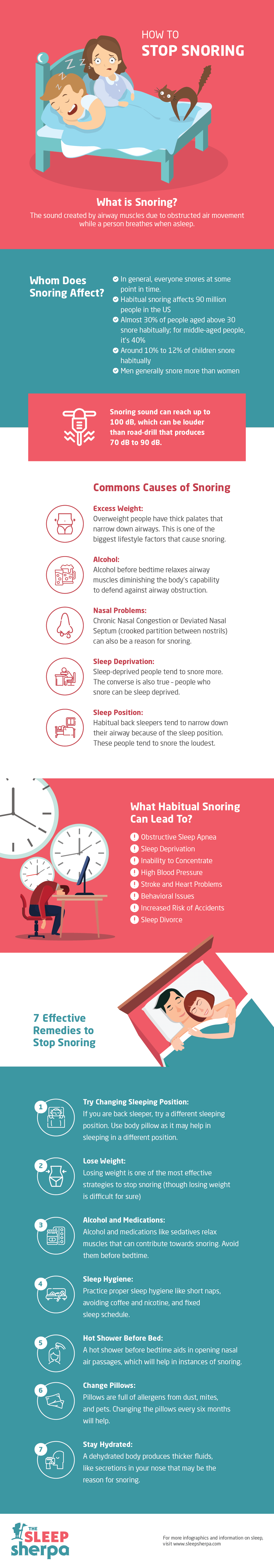
The most common type of sleep apnea, Obstructive Sleep Apnea (OSA), is characterized by repeated episodes of complete or partial obstructions of the upper airway during sleep, often resulting in reduced or completely halted airflow (2). While snoring, choking, or gasping for air during sleep, symptoms typically associated with OSA, are also seen in women, they may not always be as pronounced. These differences, coupled with the stereotyping of sleep apnea as a male disorder, contribute to underdiagnosis in women (3).
In women, the symptoms often manifest more subtly and may include insomnia, headaches, daytime fatigue, mood changes, depression, and difficulty in concentrating (4). These less overt symptoms make it more challenging to diagnose sleep apnea in women.
A critical symptom to watch for in women is insomnia, characterized by trouble falling asleep or staying asleep. While insomnia has various causes, it can also be a symptom of sleep apnea. Women with sleep apnea frequently report awakening in the night and difficulty returning to sleep (5).
Women with sleep apnea often experience morning headaches. These headaches result from decreased oxygen levels during sleep caused by the repeated cessation of breathing, leading to widened blood vessels in the brain (6).
One of the most significant signs of sleep apnea in women is excessive daytime sleepiness. Despite a full night’s sleep, women suffering from sleep apnea often wake up feeling tired and experience fatigue throughout the day. This daytime sleepiness is due to the interrupted sleep cycle caused by apnea episodes (7).
A study published in the European Respiratory Journal observed that mood changes and depression were more common in women with sleep apnea than in men (8). The constant interruption of deep sleep due to sleep apnea can have an impact on mood, leading to irritability, anxiety, and depression.
Lastly, cognitive issues like difficulty concentrating or memory loss can also be indicative of sleep apnea in women. As observed in a study published in the Journal of Clinical Sleep Medicine, these cognitive impairments result from repeated disruptions in the sleep cycle, preventing women from achieving restful, deep sleep (9).
Recognizing these symptoms is crucial, as untreated sleep apnea can lead to serious health complications like hypertension, heart disease, stroke, and diabetes (10). Early diagnosis in women, therefore, could significantly improve quality of life and reduce the risk of these comorbid conditions.
Despite the increased awareness and research, sleep apnea in women remains underdiagnosed. Raising consciousness about these less-recognized symptoms is essential to improve detection and treatment. Medical professionals should be vigilant about the possible symptoms of sleep apnea in women to facilitate early diagnosis and effective treatment.
Sources:
- Valipour, A. (2012). Gender-related differences in symptoms of patients with suspected breathing disorders in sleep: a clinical population study using the sleep disorders questionnaire. Sleep, 35(3), 363-373.
- Punjabi, N. M. (2008). The epidemiology of adult obstructive sleep apnea. Proceedings of the American Thoracic Society, 5(2), 136-143.
- Lin, C. M., Davidson, T. M., & Ancoli-Israel, S. (2008). Gender differences in obstructive sleep apnea and treatment implications. Sleep Medicine Reviews, 12(6), 481-496.
- Young, T., Finn, L., Austin, D., & Peterson, A. (2003). Menopausal status and sleep-disordered breathing in the Wisconsin Sleep Cohort Study. American Journal of Respiratory and Critical Care Medicine, 167(9), 1181-1185.
- O’Connor, C., Thornley, K. S., & Hanly, P. J. (2000). Gender differences in the polysomnographic features of obstructive sleep apnea. American Journal of Respiratory and Critical Care Medicine, 161(5), 1465-1472.
- Gelaye, B., Lohsoonthorn, V., Lertmeharit, S., Pensuksan, W. C., Sanchez, S. E., Lemma, S., … & Williams, M. A. (2015). Construct validity and factor structure of the Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale in a multi-national study of African, South East Asian and South American college students. PloS one, 10(12), e0140208.
- Antic, N. A., Catcheside, P., Buchan, C., Hensley, M., Naughton, M. T., Rowland, S., … & McEvoy, R. D. (2011). The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep, 34(1), 111-119.
- Bixler, E. O., Vgontzas, A. N., Lin, H. M., Ten Have, T., Rein, J., Vela-Bueno, A., & Kales, A. (2001). Prevalence of sleep-disordered breathing in women: effects of gender. American Journal of Respiratory and Critical Care Medicine, 163(3), 608-613.
- Twigg, G. L., Papaioannou, I., Jackson, M., Ghiassi, R., Shaikh, Z., Jaye, J., … & Morrell, M. J. (2010). Obstructive sleep apnea syndrome is associated with deficits in verbal but not visual memory. American Journal of Respiratory and Critical Care Medicine, 182(1), 98-103.
- Peppard, P. E., Young, T., Palta, M., & Skatrud, J. (2000). Prospective study of the association between sleep-disordered breathing and hypertension. New England Journal of Medicine, 342(19), 1378-1384.

Sleep Apnea Treatment Options for Women
Sleep apnea, a condition that results in interrupted breathing during sleep, has been identified as a major health concern affecting an increasing number of women. Left untreated, sleep apnea can lead to severe health complications, including cardiovascular diseases, stroke, and diabetes (1). Fortunately, a number of effective treatments are available that can significantly improve the quality of life for women suffering from this sleep disorder.
The first line of treatment for Obstructive Sleep Apnea (OSA), the most common type of sleep apnea, often involves lifestyle modifications. These include weight management, reducing alcohol consumption, cessation of smoking, and avoidance of sedative medications. Obesity is a significant risk factor for OSA, and weight reduction has been found to alleviate the symptoms significantly in numerous studies (2).
Sleep position can also influence OSA severity. It’s been reported that sleep apnea is often worse when sleeping on the back (supine position) due to the effect of gravity on the airway. Therefore, positional therapy, which encourages sleeping on the side, could be beneficial for some women (3).
For moderate to severe sleep apnea, Continuous Positive Airway Pressure (CPAP) therapy is commonly prescribed. This involves wearing a mask over the nose and/or mouth during sleep. The device gently blows air into the airway to keep it open and prevent apneas (4). Although it can take some time to adjust to the treatment, it is highly effective when used consistently.
Beyond CPAP, there are other types of positive airway pressure devices such as BiPAP (Bilevel Positive Airway Pressure) or ASV (Adaptive Servo-Ventilation), which can be used depending on the patient’s needs and how they respond to therapy (5).
Oral appliances designed to keep the throat open, such as mandibular advancement devices, can also be an effective treatment option for some women. These devices, which look like sports mouth guards, help to keep the airway open by holding the tongue or jaw forward to ease airflow during sleep (6).
In certain cases, surgical options may be explored. A variety of procedures can be done depending on the cause of the sleep apnea, including nasal surgery, throat surgery, or oral surgery. In some cases, more than one procedure may be performed (7).
New treatments are continually being developed and tested. Hypoglossal nerve stimulation is a newer surgical treatment that stimulates a nerve in the chest to keep the airway open during sleep. Clinical trials have shown promising results in reducing the symptoms of sleep apnea (8).
Finally, it is crucial to remember that regular follow-ups with healthcare professionals and sleep specialists are necessary once treatment is initiated. This will ensure the most effective treatment is being used and adjusted as necessary for each individual.
Treating sleep apnea is essential to prevent long-term health problems. Women with sleep apnea symptoms should consult their healthcare provider for a thorough evaluation and to discuss the best treatment options for their individual situation.
Sources:
- Peppard, P. E., Young, T., Palta, M., & Skatrud, J. (2000). Prospective study of the association between sleep-disordered breathing and hypertension. New England Journal of Medicine, 342(19), 1378-1384.
- Tuomilehto, H., Seppä, J., Uusitupa, M., Peltonen, M., Martikainen, T., Sahlman, J., … & Gylling, H. (2013). The impact of weight reduction in the prevention of the progression of obstructive sleep apnea: an explanatory analysis of a 5-year observational follow-up trial. Sleep Medicine, 14(8), 769-775.
- Cartwright, R. D. (1984). Effect of sleep position on sleep apnea severity. Sleep, 7(2), 110-114.
- Sullivan, C. E., Issa, F. G., Berthon-Jones, M., & Eves, L. (1981). Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. The Lancet, 317(8225), 862-865.
- Morgenthaler, T. I., Kagramanov, V., Hanak, V., & Decker, P. A. (2006). Complex sleep apnea syndrome: is it a unique clinical syndrome?. Sleep, 29(9), 1203-1209.
- Marklund, M., Verbraecken, J., & Randerath, W. (2020). Non-CPAP therapies in obstructive sleep apnoea: mandibular advancement device therapy. European Respiratory Journal, 55(4).
- Sher, A. E., Schechtman, K. B., & Piccirillo, J. F. (1996). The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep, 19(2), 156-177.
- Schwartz, A. R., Bennett, M. L., Smith, P. L., De Backer, W., Hedner, J., Boudewyns, A., … & Anderson, P. (2001). Therapeutic electrical stimulation of the hypoglossal nerve in obstructive sleep apnea. Archives of Otolaryngology–Head & Neck Surgery, 127(10), 1216-1223.
Sleep Apnea in Transgender Women: Recognizing the Risk and Seeking Effective Solutions
Recent research suggests that transgender women may be particularly vulnerable to this condition. Understanding the unique challenges and risk factors faced by transgender women in relation to sleep apnea is essential for healthcare professionals to provide appropriate diagnosis, treatment, and support. In this article, we delve into the topic, shedding light on the connection between sleep apnea and transgender women while emphasizing the importance of early detection and tailored interventions.
Exploring the Risk Factors:
Transgender women, individuals assigned male at birth but identifying and living as women, face a range of factors that can contribute to their increased susceptibility to sleep apnea. While not exclusive to this population, these factors may include hormonal therapies, obesity, and anatomical variations. It is crucial for medical practitioners to recognize these risk factors and be aware of the potential impact they may have on a transgender woman’s sleep health.
Hormonal Therapies and Sleep Apnea:
Hormonal therapy, a common aspect of gender-affirming care for transgender women, involves the use of estrogen and anti-androgen medications to promote feminization and suppress male characteristics. While these therapies are crucial for gender affirmation, they can potentially affect sleep patterns and contribute to sleep apnea development. Studies suggest that hormonal therapies may lead to changes in upper airway muscle function, increasing the risk of airway collapse during sleep and subsequent apnea episodes.
Obesity and Sleep Apnea:
Obesity, a well-known risk factor for sleep apnea, is prevalent among both cisgender and transgender populations. However, transgender women may face additional challenges due to factors such as hormonal therapies, which can contribute to weight gain or make it more difficult to lose weight. Obesity can exacerbate sleep apnea symptoms, as excess weight around the neck and throat can narrow the airway and obstruct breathing during sleep. Addressing obesity and promoting healthy lifestyle choices should be a crucial part of comprehensive care for transgender women with sleep apnea.
Anatomical Variations and Sleep Apnea:
Another consideration is the potential impact of anatomical variations on the development and severity of sleep apnea in transgender women. While research in this specific area is limited, studies have shown that transgender women may have anatomical differences in their upper airway compared to cisgender individuals. These differences may increase the risk of airway collapse and subsequent apnea episodes during sleep. Further investigation is needed to fully understand the extent to which anatomical variations contribute to sleep apnea in this population.
Sleep Apnea in Men vs. Women
According to the American sleep apnea Association, men are two to three times more likely to have sleep apnea than women. However, researchers believe that the actual disparity may be smaller due to underdiagnosis in women. Indeed, the symptoms exhibited by women often diverge from the ‘classic’ signs of sleep apnea – loud snoring, gasping or choking during sleep, and excessive daytime sleepiness – which are more commonly observed in men.
In contrast to men, women with sleep apnea may present with less noticeable symptoms such as insomnia, morning headaches, mood disturbances, and fatigue, which can often be mistaken for signs of other health issues like depression, menopause, or chronic fatigue syndrome. This discrepancy in symptoms can lead to a significant delay in diagnosis and treatment for women, with potential implications for their long-term health.
A man’s risk of developing sleep apnea rises with age, particularly after 40, and is further increased if he is overweight or has a family history of the disorder. Conversely, premenopausal women have a lower risk, likely due to the protective hormonal effects of estrogen and progesterone. However, this risk escalates after menopause, equalizing the odds between the sexes in later life.
The outcomes and consequences of sleep apnea also differ between men and women. Men with untreated sleep apnea have been found to be at a higher risk of heart problems and strokes. On the other hand, women with untreated sleep apnea are more likely to suffer from depression and anxiety, reduced quality of life, and poor cognitive function. Alarmingly, women with sleep apnea also show a faster cognitive decline than their male counterparts.
These gender-based differences in sleep apnea are not merely academic curiosities; they are vital clues that can guide personalized treatment strategies. They underline the importance of gender-specific research and tailored approaches to diagnosis, which can help to bridge the gap in care and offer effective treatment for all patients.
When to Speak to a Doctor About Sleep Apnea
Sleep apnea is a serious sleep disorder that can have profound implications on your health if left untreated. With potential effects ranging from diminished quality of life to heightened risk of cardiovascular diseases, it’s critical to seek medical help if you suspect you might be suffering from this condition. But when exactly should you raise your concerns with a doctor? Here are the key signs to watch out for.
The most characteristic sign of sleep apnea is chronic and loud snoring punctuated by pauses, followed by choking or gasping sounds. However, it’s important to remember not everyone who snores has sleep apnea. It’s the pattern of interrupted breathing that raises the red flag.
Daytime symptoms are equally significant. Do you often wake up feeling unrefreshed despite getting a full night’s sleep? Excessive daytime sleepiness, despite adequate sleep time, is a common symptom of sleep apnea. It can leave you feeling chronically fatigued and unable to concentrate, impacting your daily activities and overall productivity.
In line with this, if you frequently wake up with a headache, it might be more than just a poor night’s sleep. Morning headaches are common in individuals with sleep apnea due to the repeated drops in oxygen levels during the night that cause blood vessels to expand.
Pay attention to your mood as well. Mood changes, such as irritability, depression, or anxiety, can also be indicative of sleep apnea. The ongoing lack of restful sleep can severely affect your mood and emotional well-being.
The presence of risk factors should also prompt a conversation with your doctor. If you are male, overweight, over the age of 40, have a neck circumference greater than 17 inches, or a family history of sleep apnea, you are at a higher risk. For women, the risk increases after menopause.
Moreover, if you have been told by your partner that you have periods of stopped breathing during your sleep, it’s crucial to discuss this with your doctor. This sign is perhaps the most indicative of sleep apnea and should not be overlooked.
Sleep apnea is not a condition to be taken lightly. If you’re experiencing any of these symptoms or have multiple risk factors, you should schedule a consultation with your doctor. They can refer you to a sleep specialist or order a sleep study to confirm the diagnosis. Remember, the sooner you seek help, the sooner you can get on the path to better sleep and improved health.